Chronic prostatitis is one of the most common diseases in adult men. Prostatitis significantly reduces quality of life, becoming a cause of mental and sexual disorders. The lack of complete information about the nature of the disease makes the treatment of chronic prostatitis a difficult task, requiring the patience of both the patient and the doctor.
Prostatitis is an inflammatory degenerative lesion of the prostate gland.
Classify
The National Institutes of Health (NIH USA) has developed and proposed a classification of chronic prostatitis as follows:
- chronic bacterial prostatitis;
- chronic non-bacterial prostatitis (with and without signs of inflammation);
- Asymptomatic chronic prostatitis.
Modern male researchers adhere to this classification in the diagnosis and treatment of inflammatory prostate diseases. Acute prostatitis stand out separately. Once a doctor knows what type of pathology is identified, the doctor will be able to select the optimal treatment regimen and achieve considerable success in treatment.
Causes and risk factors
The division into chronic bacterial and non-bacterial prostatitis is not accidental. Different causes of the disease determine treatment strategies and largely influence the outcome of the disease.
Chronic bacterial prostatitis
Chronic bacterial prostatitis occurs in 10-15% of patients. The immediate cause of the development of the disease is the infiltration of the pathogenic flora and the opportunity to enter the prostate gland. By definition, the prostate gland is free of bacteria. Prostate infection can be through the urethra, as well as through blood and lymph. During the examination, the following microorganisms are most commonly detected:
- Escherichia coli (up to 95%);
- Proteus;
- klebsiella;
- pseudomonas.
Representatives of the gram-positive flora (staphylococci, streptococcus) are quite rare. In some cases, growth of two or more microorganisms is noted (mixed infection). It is possible to become infected with pathogenic bacteria (chlamydia, Trichomonas, gonococcus and others).
Most of the microorganisms detected during the examination are representative of the normal microflora. Under normal conditions, they are harmless to the body and exist peacefully on the mucous membranes of the urinary system and gastrointestinal tract. Under certain conditions, growth and reproduction of pathogenic flora occur, leading to inflammation of the prostate tissue and the appearance of all symptoms of the disease.
Risk factors for developing chronic bacterial prostatitis:
- do not comply with personal hygiene;
- Hypothermia;
- genital injury;
- inflammatory diseases of the urinary system;
- presence of STIs.
All of this leads to a decrease in local and general immunity and the natural reproduction of the prostate flora. It is not excluded that infections that can penetrate the urethra in inflammatory genital diseases. The likelihood of prostatitis increases with existing urethritis, cystitis, and colitis.
Chronic non-bacterial prostatitis
There are several theories about the appearance of this form of the disease:
- Chemical inflammatory theory. . . Throwing urine into the prostate gland during urination leads to deposition of urate and the development of inflammation. Prostate-urethral reflux is facilitated by narrowing of the urethra (constriction) and other developmental abnormalities.
- Immunological theory. . . Version based on autoimmune damage to prostate tissue resulting from exposure to bacterial antigens. Genetic dispositions for this form of pathology are considered.
- Neurobiological theory. . . Violation of the viscera in the pelvic region causes stagnation of blood in the organs and leads to the development of prostatitis.
In the development of non-bacterial prostatitis, the following risk factors also need special attention:
- long-term sedentary work;
- sedentary lifestyle;
- bad habits;
- stress and emotional overload;
- prolonged sexual abstinence.
These risk factors provoke the development of an obstruction in the prostate gland, leading to a violation of the pelvic organs. Microbiological factors only play a role in the early stages of the development of the disease. In the future, its importance diminishes, and autoimmune processes and nutritional disorders in the tissues of the prostate appear first.
According to statistics, 85-90% of men suffer from non-bacterial chronic prostatitis (not directly related to a pathogenic or opportunistic bacterial infection).
The symptoms
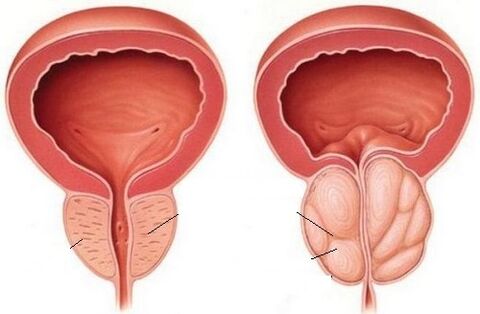
Chronic prostatitis occurs mainly in men aged 25-40 years. With age, the likelihood of having the disease increases. In the old age, prostatitis is often associated with adenoma - a benign tumor of the prostate gland.
Signs of chronic prostatitis:
- dull pain in the lower abdomen;
- radiograph pain in the groin, scrotum, perineal, lower back, sacrum;
- Increased discomfort during intercourse and during bowel movements.
Very characteristic urination disorders:
- frequent urination;
- excretion of urine in small portions;
- inadequate feeling of the bladder;
- the appearance or intensification of pain during urination;
- Slow and interrupted urine flow.
The following symptom is characteristic of prostate adenoma, often occurring against the background of chronic prostatitis.
With a long course of the disease, there are disorders in the sexual sphere:
- decreased libido;
- impaired erection ability;
- reduce the time of intercourse;
- premature ejaculation;
- pulling pain in the lower abdomen after ejaculation;
- lack of a spontaneous morning erection.
Chronic prostatitis is one of the leading causes of erectile dysfunction, in which the man is unable to achieve and maintain a sufficient erection for a full sexual intercourse. Such a condition significantly disrupts the course of life, which can cause depression and other psychological disorders.
Asymptomatic chronic prostatitis occurs without any clinical manifestations. The disease was discovered by accident when examined by a urologist. Although there are no symptoms, prostatitis can lead to serious complications, erectile dysfunction, and other health problems.
Complications
The advent of prostatitis causes the development of such conditions:
- prostate abscess;
- cystitis and pyelonephritis (cystitis and kidney inflammation);
- cholecystitis (seminal vesitis);
- erectile dysfunction;
- dry.
The earlier the disease is detected and treatment is started, the more chance there is for a favorable outcome of the disease.
Diagnose
The following methods are used to detect chronic prostatitis:
Checked by a urologist
At an individual appointment, the doctor focuses on the patient's complaints. The external genitals are examined, and a digital rectal examination of the prostate gland is performed. When palpating, the doctor assesses the size and shape of the gland. In the case of chronic prostatitis, this organ will be slightly enlarged. The procedure is combined with the collection of prostate secretions for microbiological examination.
Sample four cups
The main method allows you to identify the inflammatory process in the prostate gland and differentiate it from other diseases. Document collection takes place in many stages. In the morning, after 5-6 hours of abstinence from the toilet, a man pee in two vials - for the first (initial) and for the second (middle) portion of the urine. In the first part, the substances contained in the urethra are washed away, in the second part - the bladder. The third part of the urine is collected after prostate massage and allows you to evaluate the condition of the prostate gland. The bile of the prostate gland is collected separately for bacterial culture.
In urine analysis, two parameters are evaluated: the number of leukocytes and the erythrocyte. With prostate disease, the number of leukocytes increases in the third part of the urine. Typically, their number does not exceed 10 in the field of view.
Microbiological examination
When conducting a tri-glass test, not only assess the number of leukocytes, but also take materials for bacterial culture. If you suspect chronic prostatitis, your doctor is particularly concerned with the third part of your urine. Based on the examination results, the doctor can identify the causative agent and select the optimal antibiotic therapy.
The identification of opportunistic bacteria in groups of 10 or more has diagnostic value.3CFU / ml or detect pathogenic microorganisms in any amount.
Bacteriological culture of prostate secretions

Inoculation of bacteria into the prostate fluid helps to assess the nature of the process (infectious or not) and to determine the type of pathogen.
Before taking the third part of the urine during prostate massage, the doctor will take the secretions secreted to check for bacteria. The results also help determine diagnostic and treatment strategies.
Diagnostic criteria for chronic bacterial prostatitis:
- Detection of opportunistic microorganisms in the third part of prostate or urine excretion at a level above 103CFU / ml.
- Detection of opportunistic bacteria in the third part of urine or prostate excretion, the amount of which is significantly higher (10 times) than in the second part of urine.
- Identify pathogenic microorganisms in the third part of prostate or urine excretion.
Supersonic
Ultrasound examination allows you to evaluate the size of the organ and identify the pathology at the same time. Most often, chronic prostatitis is associated with prostate adenoma - a benign tumor.
The principles of treatment
The goal of therapy for chronic prostatitis is to eliminate the inflammatory process, activate blood flow and improve the nutrition of the organs. When pathogenic or opportunistic microorganisms are detected at a high price, they are rejected. Pay special attention to regulating the lifestyle and stimulating the body's defenses.
Medicine treatment
The following drugs are used to treat chronic prostatitis:
- The antibacterial drug is selected taking into account the identified pathogen.
- Anti-inflammatory drugs to reduce inflammation and pain.
- Means that facilitate urination (alpha blockers, help relax the muscles of the urethra and stimulate the outflow of urine).
- Mean increases blood flow in the pelvic organs.
The choice of an antibiotic will depend on the known pathogen. When choosing a drug, one should take into account the possibility of penetrating the hemostasis barrier and accumulation in the tissues of the prostate gland. These conditions are met by means from the fluoroquinolone group. Macrolides and tetracycline are also used to treat chronic prostatitis.
As recommended by the European Urological Association, antimicrobial therapy should last at least 2 weeks after preliminary diagnosis has been established.
After receiving the results of bacteriological research and confirming the bacteriological nature of the disease, the treatment lasts up to 4-6 weeks. This not only eliminates the pathogen, but also prevents the recurrence of prostatitis.
Unfortunately, antibiotic therapy is not always effective. Many microorganisms successfully exist in the secret of the prostate gland for a long time and are resistant to antibiotics. Bacteria form special biofilms and form microbial colonies covered with a complex polysaccharide structure. Most antibacterial drugs cannot penetrate this biological barrier, which significantly reduces the effectiveness of the therapy. This problem can be avoided by using modern antibiotics, which can not only penetrate the tissue of the prostate gland and heat it up, but also pass through the biofilm and infect the bacteria being told. such a serious defense.
Non-drug therapy
Among the non-drug treatments, massage of the prostate gland gets special attention. The procedure stimulates blood supply to the prostate gland, eliminates obstruction and facilitates secretion. The combination of massage and long-term antimicrobial use is the main way to reduce the unpleasant symptoms of chronic prostatitis for men.
Physiotherapeutic methods of influence are used in the treatment of chronic prostatitis, along with its effects. Good effects are seen from the use of ultrasonic waves, lasers, radio waves and electromechanical stimulation. Prostate shock wave massage (UHM) is very popular. Physiotherapy is specifically indicated in cases where erectile dysfunction is one of the complications of prostatitis.
Special attention should be paid to diet in the treatment of prostatitis. The following foods should be excluded from the diet:
- alcohol;
- spicy, spicy food;
- fried and fatty foods (including fatty meats and fish).
Salt intake is limited to 5 g per day. Priority for fresh fruits and vegetables, herbs. Should be steamed.
Diet will speed up the recovery process, enhance immunity and help the body cope with the stress caused by antibiotics during treatment.
Ethnographic
Not all men see a doctor when the symptoms of prostatitis appear. Typically, men prefer treatment with folk methods, using a background of knowledge from many forums, relying on the advice of friends, relatives and neighbors. Neglecting one's own health, refusing proper antibiotic therapy and other traditional methods of exposure threaten the development of complications and deterioration of the general condition. Untreated prostatitis can cause erectile dysfunction. Is it worth the risk if you can see your doctor on time and fix the problem with minimal losses?
Of course, among the methods of traditional medicine, there are several aspects that deserve special attention. Modern urology has noted the effectiveness of many herbs in the treatment of chronic prostatitis. Experts recommend herbal preparations based on the following ingredients:
- Pumpkin oil;
- green winter round leaves;
- garden parsley;
- Perfume St. John's wort;
- canadian goldenrod;
- licorice root;
- echinacea.
Separately or in combination, these ingredients stimulate blood flow in the pelvic organs, eliminate blockages and stimulate the immune system.
Phytop preparations will not eliminate the body of pathogenic bacteria, but will help eliminate the symptoms of the disease.
Combined with antibacterial drugs and prostate massage, herbal therapies significantly improve the general condition and speed up the recovery process.
Prevent
The following recommendations will help reduce your risk of developing chronic prostatitis:
- It is not allowed to hypothermia of the whole body and genital area, pelvis and lower extremities. In the cold season, wearing thermal underwear is worth discussing.
- Intimate hygiene rules should be followed and condoms used to protect against sexually transmitted diseases. The best prevention would be to refuse to have normal sex.
- You should pay attention to your health and promptly treat vaginal diseases.
- It is not superfluous if you follow a diet (give up spicy, fried and fatty foods), and keep fit (sports, exercise, walking).
All men over 30 years old should see a routine check-up by a urologist (at least once a year). If you experience any unpleasant symptoms, you should see your doctor as soon as possible.
Frequently asked questions
Can chronic prostatitis be cured?
Contrary to popular belief, chronic prostatitis can be successfully treated. If you follow all the recommendations of your doctor, you can get rid of the unpleasant symptoms of prostatitis and significantly improve your quality of life.
Can chronic prostatitis be asymptomatic?
Yes, this variant of the disease is detected only after an examination by the urologist.
Is chronic prostatitis in sexual partners dangerous for women?
Sexually transmitted infections are often the cause of chronic prostatitis. If one pathogen is identified, both partners must be treated. Otherwise, there is a risk of infection and less effectiveness of therapy due to relapse.
Can chronic prostatitis have sex?
Yes, if the general condition allows and there is no problem in the sexual field (erectile dysfunction).
Can chronic prostatitis be pregnant?
Yes, if the function of the prostate gland is preserved and its secret is fully developed. Before conception, should seek medical attention and treatment by a urologist. Infections that cause the development of prostatitis are very contagious to women. Infection in the uterus of the fetus can cause developmental abnormalities and termination of pregnancy.
How does chronic prostatitis affect potency?
Chronic prostatitis threatens the development of erectile dysfunction. With such a pathology, there is a decrease in libido, the frequency and strength of the erections decreases, orgasm becomes painful. In advanced cases, sexual activity becomes impossible.
Can chronic prostatitis be cured without antibiotics?
Antibiotic therapy is considered one of the key treatments for chronic prostatitis. In most cases, it is impossible to cope with the disease without antibiotics.
Can chronic prostatitis be cured with folk remedies?
Curing chronic prostatitis alone with traditional medicine alone will not be effective. To achieve optimum effect, complex treatment is carried out using antibiotics, herbal preparations, anti-inflammatory drugs and physiotherapy methods.



























